Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
02 Mar
Are Gut Microbiome Kits Overpromising?
The American Gut Project tests 21 at-home gut microbiome kits from seven companies and finds “major discrepancies.”
27 Feb
Depression Therapy That Usually Takes 6 to 8 Weeks May Work Just as Well in 5 Days
A new study finds transcranial magnetic stimulation, used for treatment-resistant depression, can provide significant symptom relief in just days instead of weeks.
26 Feb
Daily Aspirin Doesn’t Protect Against Colon Cancer in Average-Risk Adults
A major, new evidence review finds taking a daily aspirin has little to no benefit for people at average risk of colorectal cancer, but it can cause dangerous bleeding and possibly stroke.
FDA To Offer Cash Bonuses for Faster Drug Reviews
The U.S. Food and Drug Administration’s (FDA) chief says the agency will begin offering bonuses to drug reviewers who complete their work ahead of schedule.
Dr. Marty Makary described the effort as a pilot program during a staff meeting last week. The first quarterly bonus payments could begin going out in August, according to presen...
- HealthDay Staff HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
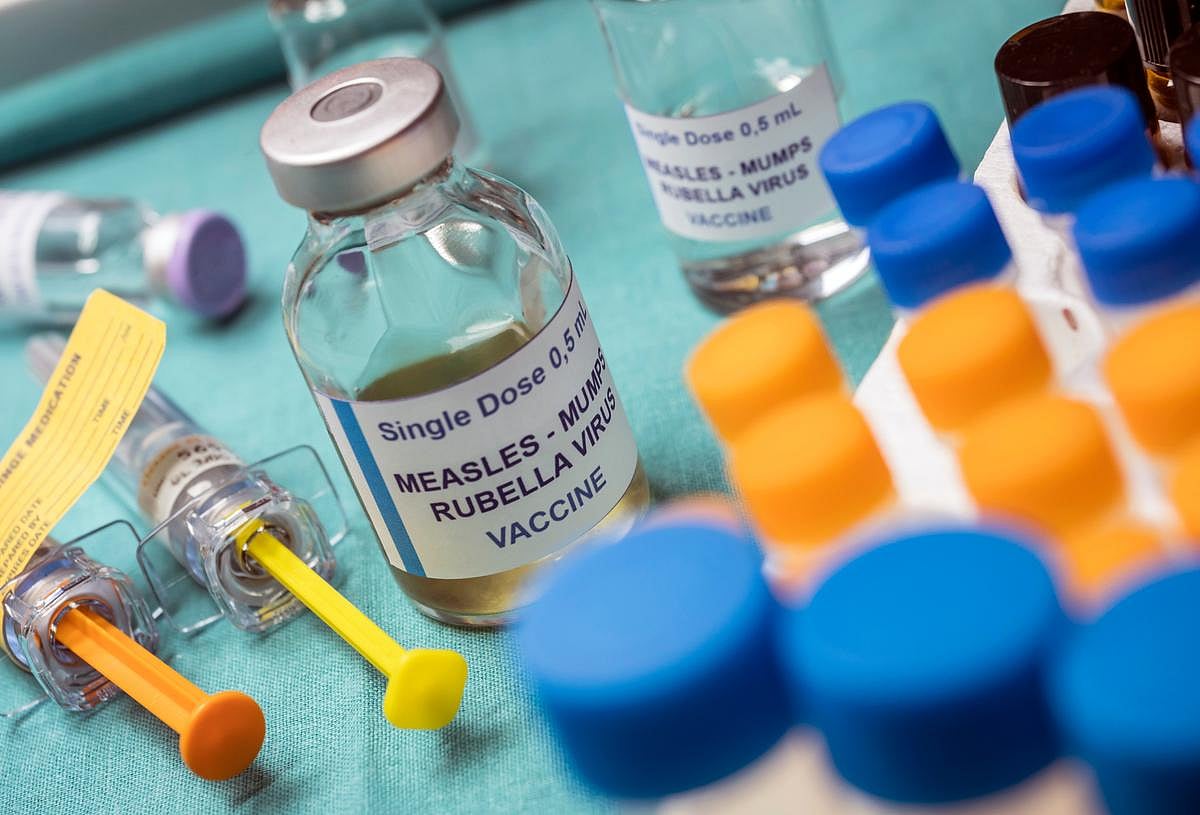
U.S. Tops 1,100 Measles Cases This Year as Outbreaks Grow
Measles cases are climbing rapidly across the United States, with more than 1,100 infections reported in the first two months of this year, data shows.
As of Feb. 26, 1,136 cases had been confirmed, according to the U.S. Centers for Disease Control and Prevention (CDC). That total is already far higher than usual numbers for an entire year...
- HealthDay Staff HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
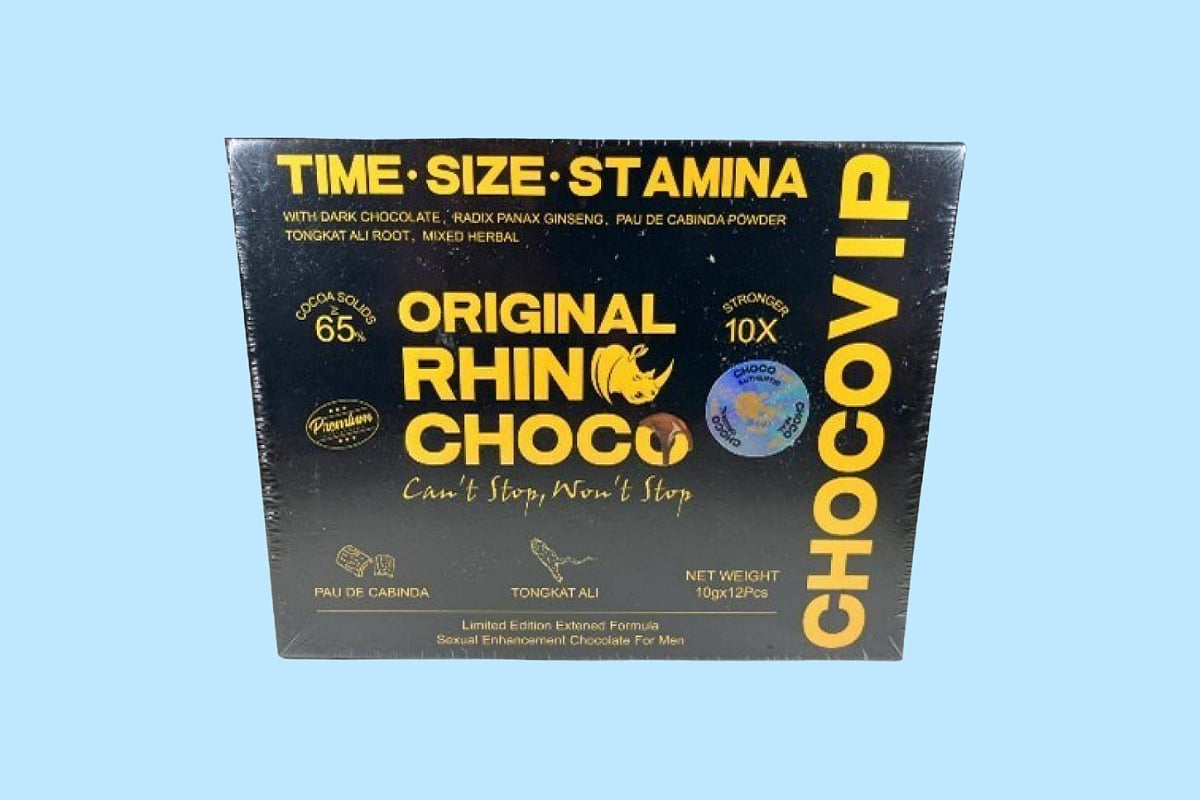
Chocolate Male Supplement Recalled Over Hidden Erectile Dysfunction Drug
A chocolate male enhancement product is being pulled from store shelves after federal health officials found it contains a hidden prescription drug.
The company — USALESS.COM, based in Brooklyn, New York — is recalling its product called Rhino Choco VIP 10X, according to an alert from the U.S. Food and Drug Administration (FDA)...
- HealthDay Staff HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
New Drug Could Boost Efforts To Wipe Out Sleeping Sickness
A new treatment for sleeping sickness could make it much easier to treat and possibly eliminate the deadly disease.
On Friday, a committee of the European Medicines Agency (EMA) recommended approval of acoziborole, a drug made by Sanofi. The decision is a key step to making the medicine available in Congo, where most cases occur, and in ot...
- HealthDay Staff HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
Telemedicine Visits Cost Five Times Less Than In-Clinic Care
Telemedicine appointments aren’t only more convenient, but actually save money for both patients and health care systems, a new study says.
Telemedicine visits are five times less costly than in-person appointments for the most common conditions, researchers recently reported in JAMA Network Open.
On average, telemedic...
- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
GLP-1 Drugs Might Ease Chronic Migraine, Study Says
Weight-loss drugs like Ozempic and Zepbound might also help people manage migraines, a new study says.
Chronic migraine sufferers taking GLP-1 drugs were about 10% less likely to need ER care for a migraine attack compared to those taking a standard first-line migraine drug, researchers are scheduled to report at an upcoming meeting of the...
- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
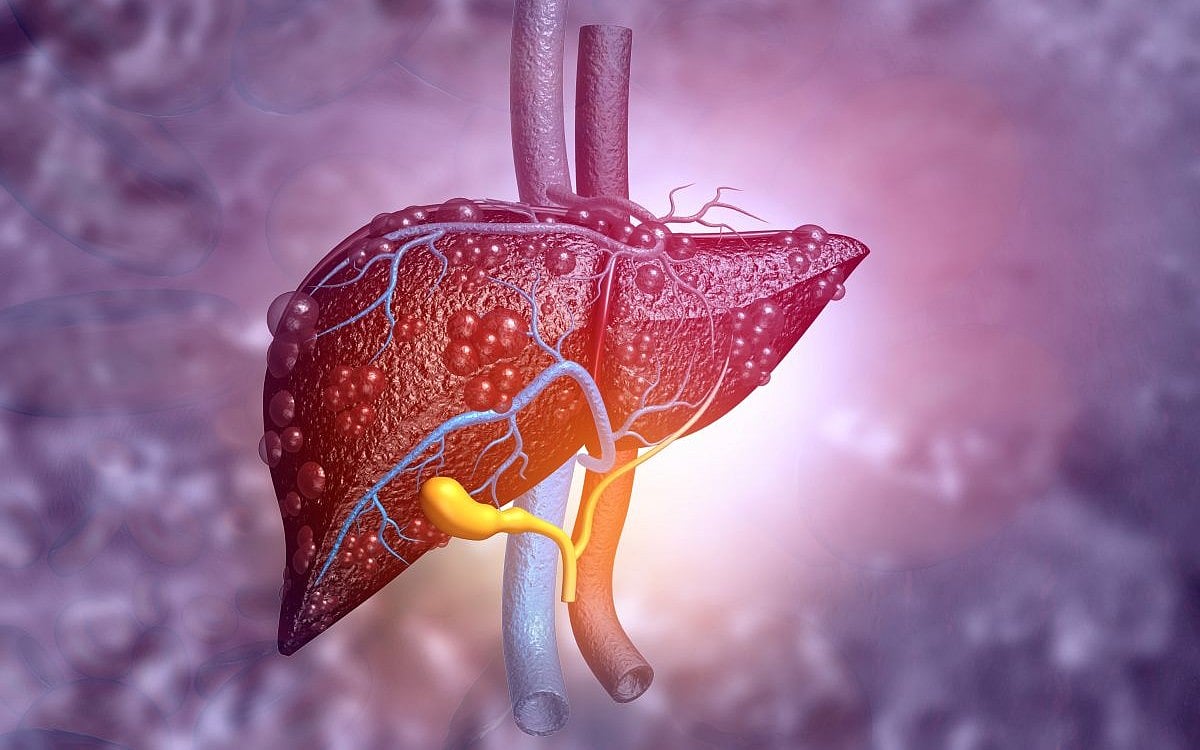
Blood Test Reveals Alcohol-Related Liver Disease
A new, easy-to-use blood test can identify when a person’s liver disease is being driven by too much drinking, researchers say.
With the test, researchers can estimate whether a person with fatty liver disease might have alcohol-related liver damage, researchers recently reported Feb. 25 in the journal Gastroenterology.
<...- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
Hormone Therapy Might Be Unnecessary For Some Prostate Cancer Patients
Some men who’ve had surgery for prostate cancer can probably skip hormone suppression therapy without harm, a new study says.
Men typically undergo radiation and hormone therapy following prostate cancer surgery to reduce the risk of their cancer coming back.
However, the hormone therapy appears to provide little survival benef...
- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
Urban Traffic Noise Disrupts Sleep, Affects Heart Health After One Night
The nighttime sounds of the city streets can jangle a person’s nerves and affect their heart health, a new study says.
People trying to sleep through the sounds of urban traffic for just one night showed signs of heart stress and impaired blood vessel function, researchers reported Feb. 25 in the journal Cardiovascular Research
- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
Benzodiazepine Use Down In U.S., But OD Risk Remains, Study Says
Benzodiazepine prescriptions have decreased in the United States, mainly among middle-aged adults and seniors, a new study says.
But these drugs still pose a risk to many people, according to findings published recently in the Journal of Clinical Psychiatry.
Nearly half of patients still prescribed benzodiazepines also are t...
- Dennis Thompson HealthDay Reporter
- |
- March 2, 2026
- |
- Full Page
Electronics Pollution Pose Added Threat to Endangered Dolphins, Porpoises
Chemicals used to produce sharp images on your computer, TV and smartphone are posing threats to life under the sea.
New research shows that liquid crystal monomers (LCMs) from household electronics and e-waste can build up in tissues of dolphins and porpoises — findings that suggest other marine species may also be at risk.
"T...
- Carole Tanzer Miller HealthDay Reporter
- |
- March 1, 2026
- |
- Full Page
Flea And Tick Pills May Pose Environmental Risks, Study Finds
Giving your kitty or pup a pill to keep fleas and ticks at bay may an unintended effect on nature.
A relatively new class of meds prescribed by veterinarians in the U.S. and abroad called isoxazolines also pose a threat to insects that play vital roles in improving soil quality and recycling nutrients in the natural world, French rese...
- Carole Tanzer Miller HealthDay Reporter
- |
- February 28, 2026
- |
- Full Page
Study Suggests One Common Amino Acid May Affect How Long Men Live
A large new study suggests that higher levels of a common amino acid called tyrosine may be linked to a shorter lifespan in men.
The research, published recently in the journal Aging-US, examined whether blood levels of two amino acids, phenylalanine and tyrosine, were connected to how long people live.
Amino acids are build...
- HealthDay Staff HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
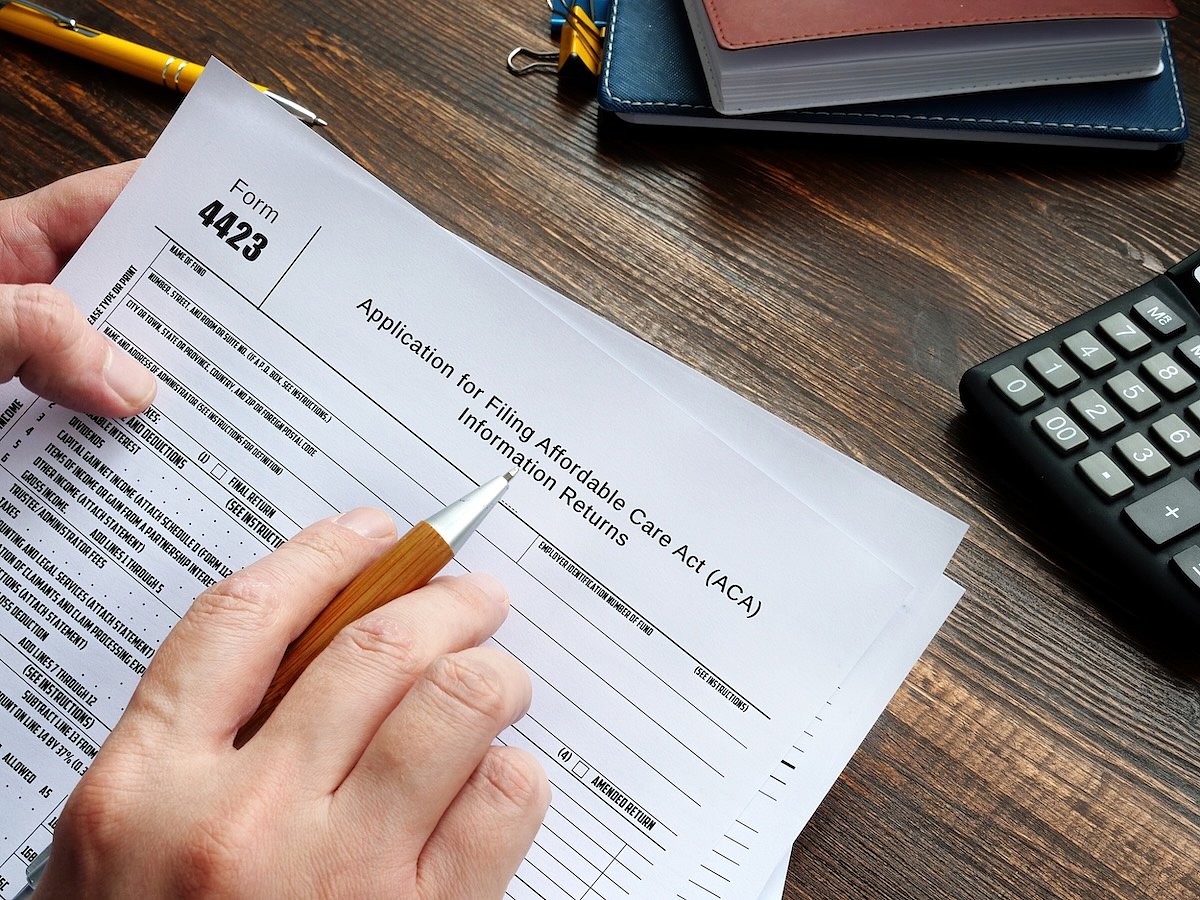
New Obamacare Rules Could Raise Deductibles to $31K For Families
The Trump administration is introducing new rules for Obamacare plans that could lower monthly premiums — but there's a catch.
They raise how much people pay out of pocket when they need care.
Under the proposed rules, some Affordable Care Act (ACA) plans would allow annual deductibles of more than $15,000 for one person and $3...
- HealthDay Staff HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Walmart Great Value Cottage Cheese Recalled Over Pasteurization Issue
Some Great Value cottage cheese products sold at Walmart are being recalled because they may not have been fully pasteurized, Saputo Cheese USA said.
The recall affects select cottage cheese products made between Feb. 17 and 20, and sold in the following states: Alaska, Alabama, Arkansas, Arizona, California, Colorado, Georgia, Iowa, Idaho...
- HealthDay Staff HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Chris Bosh Says He’s 'Lucky To Be Alive' After Sudden Health Scare
A routine evening took a terrifying turn for Basketball Hall of Famer Chris Bosh when he suddenly collapsed with no warning, he told fans this week.
The 41-year-old former NBA star shared details of the incident in a post on Instagram Wednesday.
Bosh said he was getting ready to go out with his wife when "the next thing you know," he...
- HealthDay Staff HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Crash Course Might Speed Brain Stimulation Treatment For Depression, Study Suggests
A brain stimulation therapy for depression can show results in as little as a workweek, a new study says.
Transcranial magnetic stimulation (TMS) typically requires daily clinic visits over six to eight weeks, a rather rigorous schedule for people grappling with depression.
But patients can see benefits in as little as five days if t...
- Dennis Thompson HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Wildfire Smoke Linked To Increase In Violent Assaults
It’s a fact that people become “crazy from the heat,” but a new study suggests that “crazy from the smoke” might also be a phenomenon.
Skies choked with smoke from wildfires are linked to an increase in violent assaults, a new study has found.
Assaults increased by nearly 4% in Seattle on smoke-filled da...
- Dennis Thompson HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Why Turning 19 Spikes Medicaid Loss for Millions
For most teens, turning 19 is a milestone of early adulthood. But for those relying on Medicaid, it often triggers a birthday cliff where health insurance simply vanishes.
A new study from the University of Chicago highlights a systemic issue: The moment a person is no longer classified as a child by the government, their risk of becoming ...
- Deanna Neff HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page
Blood Test Can Predict Short-Term Survival Among Seniors
An experimental blood test can predict whether seniors have long to live, a new study says.
The genetics-based blood test predicted two-year survival with accuracy as high as 86% among hundreds of seniors, researchers reported Feb. 24 in the journal Aging Cell.
The test is based on PIWI-interacting RNA (piRNA), a class of ge...
- Dennis Thompson HealthDay Reporter
- |
- February 27, 2026
- |
- Full Page