Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
23 Aug
The 14 Most Common Long COVID Symptoms in Children and Teens
A new study finds Long COVID in children impacts nearly every organ system and can be disabling for long periods of time.
22 Aug
Meat-Heavy Diet Linked to Increased Risk of Type 2 Diabetes
A new global study finds daily consumption of processed meat or unprocessed red meat significantly raises the odds of developing type 2 diabetes.
21 Aug
Smoking Just 1-2 Cigarettes a Day Before or During Pregnancy Is a Danger to Newborn Health, Study Finds
A new study suggests there is no safe time or level for smoking cigarettes before or during pregnancy.
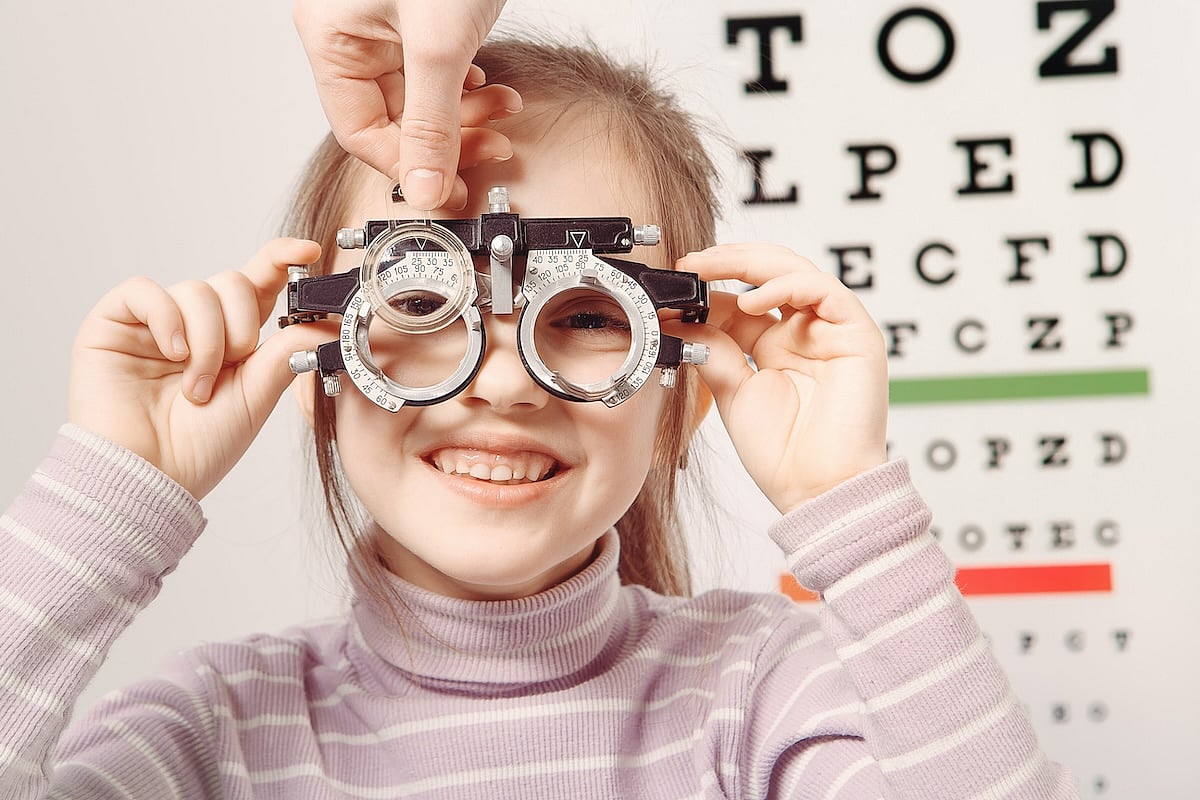
Does Your Child Need Glasses? Look for These Signs
You've noticed your young child complains of headaches and rubs their eyes a lot. Does that mean it's time to get glasses?
It could, says a Baylor College of Medicine expert, and noticing these signs early is critical for young children because their schoolwork could suffer or they could lose their vision completely.
“There is ...
- Robin Foster HealthDay Reporter
- |
- August 24, 2024
- |
- Full Page
Federal Judge Rules That U.S. Military Cannot Reject HIV-Positive Enlistees
People with HIV can no longer be turned away if they try to enlist in the U.S. military, a federal judge has ruled.
The decision, issued this week by U.S. District Judge Leonie Brinkma, said the Pentagon’s ban on HIV-positive people seeking to join the armed forces contributes “to the ongoing stigma surrounding HIV-positiv...
- Robin Foster HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Not Just Cancer: HPV May Hamper Men's Fertility
Human papillomavirus (HPV) has largely been seen as a health problem of women, given that it causes nearly all cases of cervical cancer.
But men also have reason to both fear HPV and get vaccinated against it, a new study says.
Infection with high-risk HPV strains might interfere with a man’s fertility, researchers reported rec...
- Dennis Thompson HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Could Drugs Used to Fight Cancer Also Slow Alzheimer's?
A new type of cancer drug might help treat brain diseases like Alzheimer’s, mouse studies suggest.
The drugs block an enzyme called indoleamine-2,3-dioxygenase 1 (IDO1), researchers reported.
IDO1 inhibitors are being developed as a treatment for cancers like melanoma, leukemia and breast cancer, researchers said. The drugs fig...
- Dennis Thompson HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Are 'Bed Rotting' and Other TikTok Sleep Trends Good for You?
Many young adults are experimenting with “bed rotting” and other sleep trends that have gone viral on TikTok and other social media platforms, a new poll shows.
Sleep experts say these trends likely won’t do any immediate harm, but they add that people would do better to see a doctor if they’re not getting adequate ...
- Dennis Thompson HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Wegovy Helps Patients With Heart Failure Avoid Heart Attack, Stroke
Research has already proven that the blockbuster weight-loss drug Wegovy (semaglutide) can slash a person's odds for heart attacks and strokes, and now more data from the same trial suggests that's even true for very ill patients with heart failure.
The finding also helps clear up a concern around the use of Wegovy in these patients, added...
- Ernie Mundell HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Too Much Time Watching Screens in 20s Raises Heart Attack Risk
Spend your youth glued to your phone, computer and TV and you cut your odds of making it to 60, a new study warns.
Data from a study tracking the health of more than 4,000 young adults for over 30 years found a higher odds for heart attack for those who'd spent a lot of time watching TV in their early 20s.
“Our findings sugges...
- Ernie Mundell HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Laws That Remove Guns From 'At Risk' People Save Lives
“Red flag” laws are an effective means of preventing suicide, a new study finds.
About one life was saved for every 17 times that an extreme risk protection order (ERPO) kept firearms out of the hands of a troubled individual, researchers reported Aug. 20 in the Journal of the American Academy of Psychiatry and the Law.
- |
- August 23, 2024
- |
- Full Page
No Link Found Between Migraines, Parkinson's Disease
Women who suffer frequent migraines don’t have any increased risk of developing Parkinson’s disease, finds a new study that refutes earlier research.
“These results are reassuring for women who have migraine, which itself causes many burdens, that they don’t have to worry about an increased risk of Parkinson’s...
- Dennis Thompson HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Improper Inhaler Use by People With COPD Is Common, Worsening Disease
Millions of people rely on medicines delivered by an inhaler to help manage chronic obstructive pulmonary disorder (COPD).
But a new European study finds many patients are using inhalers improperly, keeping them from adequately treating the respiratory illness.
“Misuse of inhalers is common, and in our study we found that app...
- Ernie Mundell HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
Kids' Organized Sports Are Increasingly for the Well-Off
Participation in youth sports is becoming a “haves” versus “have-nots” situation, a new study shows.
Income, education and social class are determining who can play in youth sports leagues, with the children of more privileged families more likely to hit the field or court, researchers reported recently in the journ...
- Dennis Thompson HealthDay Reporter
- |
- August 23, 2024
- |
- Full Page
FDA Approves Updated COVID Shots for Fall
Updated shots you may soon get to shield against COVID-19 infection were approved by the U.S. Food and Drug Administration on Thursday.
This year's approval for the updated mRNA vaccines comes much sooner than happened in 2023, when fall vaccines were authorized on Sept. 11.
The latest shots from Moderna and Pfizer will now target a...
- Ernie Mundell HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
Women Could Have New Medical Option to Ease Hot Flashes
A drug under development could provide a much needed option for women seeking relief from hot flashes and other menopausal symptoms, new research shows.
The drug, elinzanetant, cut the frequency of hot flashes by an average of about 56% after one month of use, and by more than 65% after three months.
Overall, about 62% of more than 3...
- Ernie Mundell HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
State Laws Strongly Affect Mental Health of Trans People, Study Finds
THURSDAY, Aug. 22, 2024 (HeathDay News) -- There's a strong association between a state's policies and laws around the rights of transgender people and the mental health of transgender residents, a new study shows.
"Trans individuals who were worried about having their rights taken away had significantly higher odds of experiencing depress...
- Ernie Mundell HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
Universal Flu Vaccine Blocks Infection in Mice
A universal flu vaccine that would protect against all influenza strains -- and that people might not need to take every year -- could be close at hand, researchers report.
An experimental vaccine candidate produced a strong immune response in lab mice, and it provided protection against severe infection after the critters were exposed to ...
- Dennis Thompson HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
Government Report Links Excessive Fluoride in Water to Lowered IQs in Kids
High levels of fluoride in drinking water may dim the intelligence of children, a new U.S. government report shows.
Based on an analysis of published research, the potentially controversial report marks the first time a federal agency has determined there is a link between drinking twice the recommended amount of fluoride and lower IQs in...
- Robin Foster HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
One Diet Might Cut Your Odds for COVID-19
COVID cases have surged this summer, but a new study suggests that following the Mediterranean diet might spare you from infection.
In a review published Wednesday in the journal PLOS One, Indonesian researchers discovered that the healthy eating regimen, which centers on fruits, vegetables, whole grains, legumes, fish a...
- Robin Foster HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
Here's What Long COVID Looks Like in Kids
Kids and teens are vulnerable to Long COVID just as adults are, with a set of distinct symptoms showing long-term health effects, a new study shows.
Ten symptoms in school-age children and 8 in teenagers indicate the likely presence of long COVID, according to findings published Aug. 21 in the Journal of the American Medical Associatio...
- Dennis Thompson HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page
Vaccination Could Shield Against Mental Issues Following Severe COVID
People stricken with a severe case of COVID-19 have a higher risk of mental illness in the year following their infection, a new study warns.
However, vaccination appears to ward off these effects on mental health, researchers reported Aug. 21 in the journal JAMA Psychiatry.
People hospitalized for COVID have a 16 times hig...
- |
- August 22, 2024
- |
- Full Page
Americans Have Mixed Feelings About AI in Health Care, Poll Finds
Most Americans believe artificial intelligence should be used to improve health care, a new national survey reports.
However, many are still a little queasy over some of the implications of widespread AI use, the poll found.
The Ohio State University survey found that most Americans think AI can be beneficial:
75% think...
- Dennis Thompson HealthDay Reporter
- |
- August 22, 2024
- |
- Full Page



.jpg?w=1920&h=1080&mode=crop&crop=focalpoint)



.jpg?w=1920&h=1080&mode=crop&crop=focalpoint)